
How trauma impacts a child’s brain
Discover how a child’s brain develops, how it responds to danger, and the long-term mental health implications of trauma.
Many young people in foster care are living with trauma, with the most common reasons for children entering care reported as abuse and neglect.
Trauma in children can have a profound and long-lasting effect on their brain development and the way in which it functions.
In this article, you’ll learn:
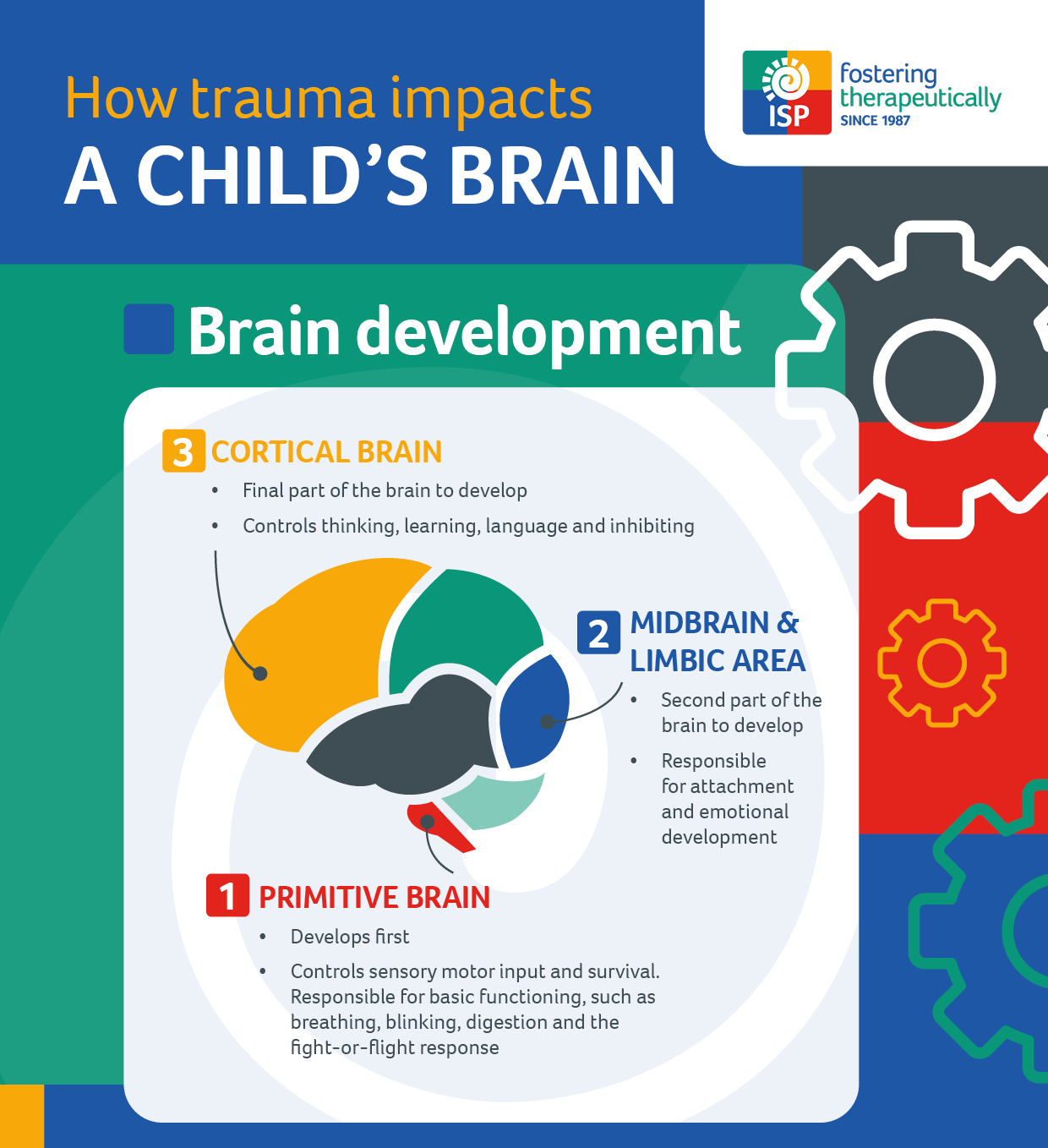
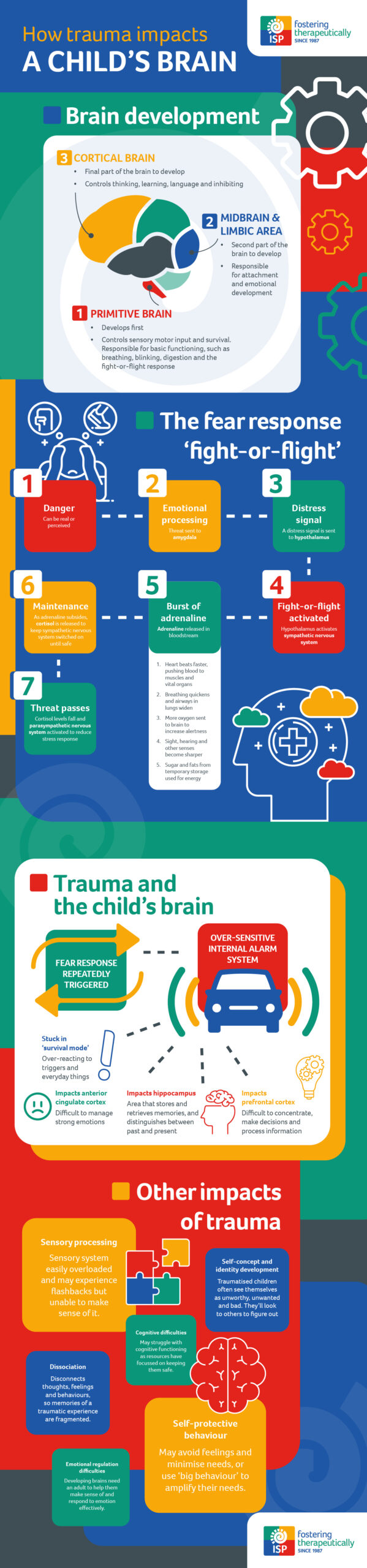
Brain development in children
The brain develops in a ‘bottom-up’ sequence. The lower parts develop first and they control the functions we do without thinking, like heartbeat, blood pressure and fight-or-flight responses.
Then the higher parts of the brain develop throughout childhood and adolescence, and are responsible for more sophisticated functions, such as empathy, emotional regulation, and cause-and-effect thinking.
Read more about the different child brain development stages below:
Primitive brain – also known as the ‘brain stem’
- First part of the brain to grow
- Already significantly developed by the end of the second trimester
- It’s the instinctual part of the brain which controls sensory motor input and survival
- Responsible for basic functioning such as breathing, blinking, digestion, fear response, and producing strong reactive states, such as anger and fear
- Before a baby is born, their brain is already adapting to the anticipated conditions in which they’ll need to survive
Midbrain and limbic area
- Second part of the brain to develop
- Responsible for attachment and emotional development
Cortical brain
- Final part of the brain to develop
- Grows rapidly in the first 3 years of a child’s life and continues to develop significantly into adulthood
- Controls thinking, learning, language and inhibiting
HOW THE BRAIN RESPONDS TO DANGER – THE FEAR RESPONSE
Our brains have a wonderful ability to protect us from danger. It’s a primal function that has evolved to keep us alive, and can be a useful physiological response in the right scenario.
Let’s take a look at what happens in our bodies when we sense danger…
Sense danger
We see, hear or sense danger.
Emotional processing
This information is immediately sent to the amygdala – the part of the brain that is responsible for emotional processing.
Distress signal
The amygdala sends a distress signal to the hypothalamus – the part of the brain that controls the fight-or-flight response.
Burst of adrenaline
The hypothalamus activates the sympathetic nervous system to release adrenaline to the bloodstream, triggering the ‘fight-or-flight’ response. Physiological changes include:
– Heart beats faster, pushing blood to the muscles, heart and vital organs
– Pulse rate and blood pressure increase
– Breathing quickens and the airways in our lungs widen, so they can take in as much oxygen as possible
– More oxygen is sent to the brain to increase alertness
– Sight, hearing and other senses become sharper
– Blood sugar and fats from temporary storage flood into the bloodstream, supplying energy to all parts of the body
Maintenance
As the initial surge of adrenaline subsides, the hypothalamus activates the HPA axis to maintain a regular release of cortisol (the stress hormone) so that the sympathetic nervous system can remain switched on until the threat passes.
Threat passes
Once the threat passes, cortisol levels fall and the parasympathetic nervous system is activated to reduce the stress response and allow the body to return to normal.
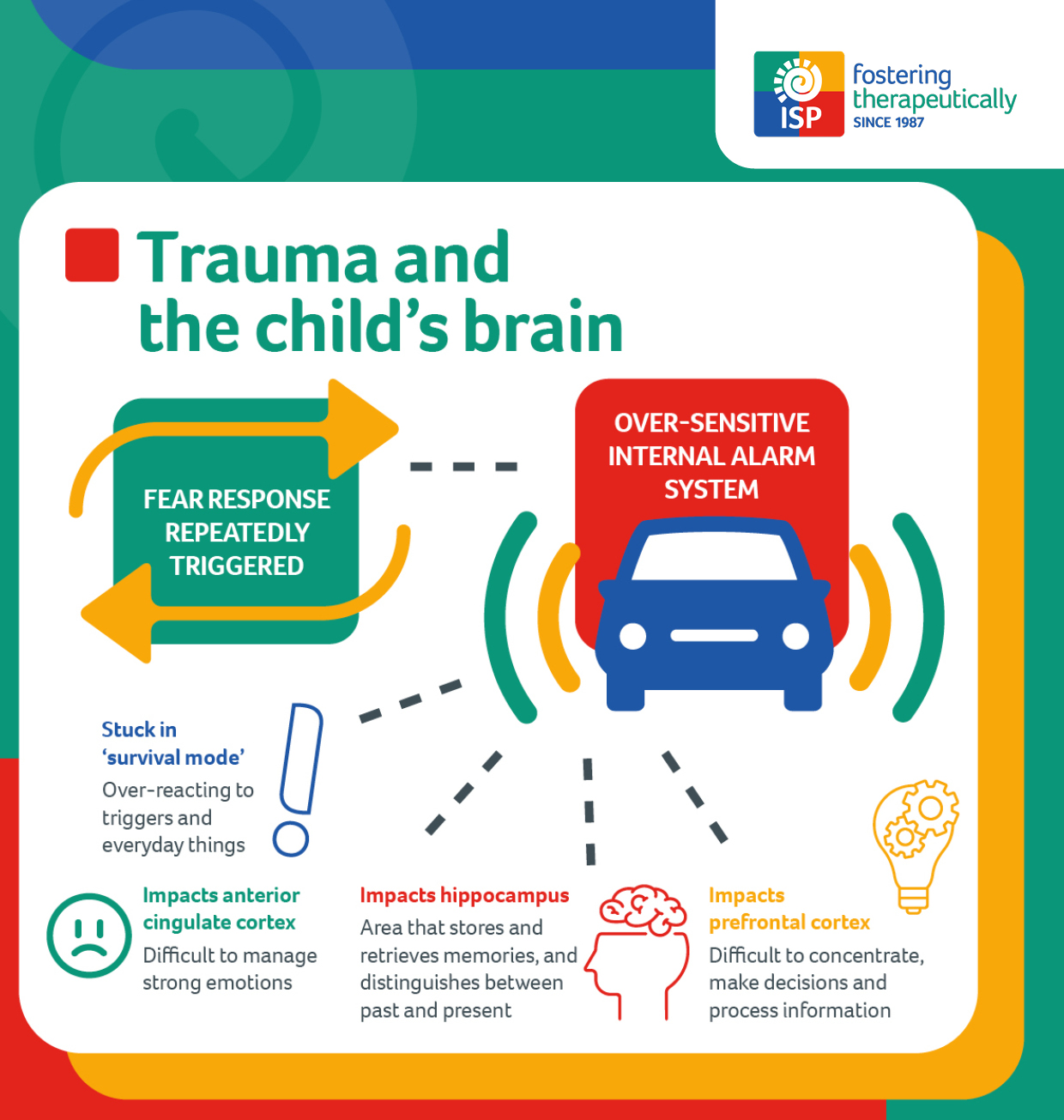
How does trauma affect a child’s brain?
When faced with a threat – whether it’s real or perceived – our brains shut down all non-essential systems and activate the fear response. The ‘primitive brain’ takes control, switching our bodies into survival mode.
In normal circumstances, the parasympathetic nervous system will kick in once the threat has passed, allowing all three parts of the brain to begin to function again. However, this is not always the case for children who are living with trauma.
Trauma causes the brain to adapt to survive
When the stress response is triggered repeatedly over a prolonged period of time, for example when a child has experienced abuse and neglect, it physically alters the brain, leaving certain parts rewired – adapted for surviving danger.
The amygdala (aka ‘the fear centre’) of a child living with trauma is likely to be in overdrive, constantly signalling danger, releasing cortisol and priming them for fight, flight, freeze or fawn responses.
This can leave the child feeling unsafe, fearful, irritated, and extremely sensitive to small everyday things such as a slightly raised voice or a classroom move. They may feel numb or not in contact with the here and now, they may redouble efforts to keep themselves feeling safe by anticipating and meeting the perceived needs of important people around them.
As well as causing elevated stress responses, trauma can also change the way the prefrontal cortex (aka ‘the thinking centre’) functions. This can make it more difficult to concentrate, make decisions and process new information. Similarly, brains which have adapted to danger may function differently in the anterior cingulate cortex (aka ‘the emotional regulation centre’), so managing strong emotions can be challenging.
Studies have also shown that trauma can impact the hippocampus – a vital part of the brain that stores and retrieves memories, as well as distinguishes between past and present events. Therefore, traumatic memories can replay in a child’s mind and seem like the threat is current, even if the memory happened in the past and the child is safer now. Triggers for these memories could be anything from a sound, smell, environment or situation to an image, movement, facial expression or touch.
Hyper v hypo arousal – the different fear responses
We often find that children who have experienced trauma struggle to be here and now, and spend a lot of time in either a heightened or numbed state. Their past traumatic experiences mean that their brains have adapted to danger and developed differently, and are very sensitive to perceived threats.
Children who have survived through fight, flight or fawn responses may continue to exist in ‘hyper-aroused states. We might notice clues that they are experiencing these states if they are running, hitting, screaming, shouting, biting, spitting, saying hurtful words, avoidance, squirming and disrupting. Their heart rate might quicken, their appetite might reduce, they might sweat and shake, and their muscles will become primed to run. Alternatively, they may show signs of heightened anxiety, panic, obsessive or compulsive behaviours, or excessively attempt to please and placate others.
Children who have survived through freeze responses (also known as ‘hypo-aroused’) are more likely to appear to shut down. Their heart rate and breathing might become slower. They may go numb, feel empty, zone out, and struggle to connect or think, make themselves physically smaller or less conspicuous
When a child is in one of these states, their behaviour is completely out of their control. The stress hormone, cortisol, is filling their body and they are stuck in their ‘primitive brain’ in ‘survival mode’. All their resources are being used up on staying alive, and so they are not able to access the higher parts of the brain where they would be able to think, reason and rationalise, draw on past learning, connect and relate to others.
Other Impacts of Trauma
Trauma impacts children in other ways too – some of these are ways in which trauma directly impacts the brain, others are ways in which a child adapts to remain safe.
Sensory processing difficulties
Hyper-vigilance can reduce a child’s ability to filter out irrelevant sensory experiences, such as background sights, sounds and textures. This can overload their sensory system, leaving them feeling overwhelmed and unsafe. They may also experience sensory flashbacks, which can involve intense feelings or physical sensations of a traumatic experience, but are unable to make sense of it or communicate what happened.
Dissociation
When an experience is completely unbearable, a child may mentally ‘leave the room’. This is a survival mechanism that disconnects thoughts, feelings and behaviours. As the memories of the traumatic experience are so fragmented, flashbacks can be confusing and they may be left unable to piece together what happened or why they might be feeling a certain way.
Self-protective strategies
Children who have experienced traumatic experiences may develop self-protective behaviour strategies or information processing patterns that enable them to survive.
For example, a baby who is completely ignored when they cry and doesn’t have their needs met, or are shouted at, shaken or hit, may learn to suppress their feelings and disconnect from their body.
A baby whose cry sometimes gets a response and other times does not, will not learn the order to how things happen due to the unpredictability of the response (i.e. when I cry, mum or dad will soothe me). They may rely on amplifying their feelings to get their needs met.
You can learn more about these strategies in the Dynamic-Maturational Model of Attachment and Adaptation (DMM) model.
Emotional regulation issues
For children who have experienced trauma, the part of the brain that regulates emotion is likely to have been significantly impacted by poor experiences of others emotional states, and of the way in which others respond to the childs emotional states.
In order to develop the capacity to regulate emotion, developing brains need an adult to help them make sense of and respond to emotion in a compassionate and effective way. If early opportunities are missed it is possible to support later development in the same way, though it takes much more time, consistency, and perseverance from trustworthy adults.
Cognitive difficulties
Children who have experienced trauma might struggle more with cognitive functioning. This is because their brains have had to be so consumed with keeping them safe and figuring out whether adults can be trusted or not, that there are less resources available for the cortical brain.
Self-concept and identity development
This starts to form from the very first messages we receive from our parents and caregivers. Many children in care see themselves as unworthy, unwanted and bad, because they have been treated as if they are, and continue to believe it’s how they think others around them see them too. They may find themselves feeling really lost, looking to others around them to figure out who they are and what they like, and try to fit in with their peers.
Many parts of a child’s identity come from birth family – their appearance, culture, religion, musical taste, and so much more. Being in foster care can put a child at a disadvantage in terms of figuring out who they are.
Trauma can be healed
The positive news is that with the right intervention at the right time, trauma recovery is possible. Just as traumatic events forge neural pathways, so can positive and therapeutic fostering experiences too.
Children are incredibly resilient and adaptable, and so with professional support and a secure attachment, over time we’re able to re-wire a child’s brain so they can live in a more stable and harmonious state.

Could you foster a child?
Many children in care have experienced early childhood trauma. Could you provide them with a stable, loving home?
We provide all of our foster parents with first-class support and access to a wide range of specialist training courses (including trauma and the brain), equipping them with the skills and knowledge they need to make a life-changing difference.
Foster Parent Training
Our free foster care training hub is designed to support you while you’re fostering.
Children With Complex Needs
We have designed a series of articles to help you care for children with complex needs.
Understand Identity
Understanding who we are and how we fit into the world around us is important.
Therapeutic Fostering
Discover more about the therapeutic fostering approach and why we founded it.
Learn about trauma…

The impact of trauma
Discover the impact of early childhood trauma, and what it means for young people in foster care.

Trauma and the brain
Learn about the profound impact that childhood trauma can have on brain development.

Healing from trauma
Explore the strategies and therapeutic perspectives you need to help children recover from trauma.